35 year old male came to the casualty with c/o fever since 4days and SOB since 1day
“This is an online e log book to discuss our patient’s de- identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patient’s clinical problems with collective current best evidence based inputs. This e-log book reflects my patient centered online portfolio and your valuable inputs on the comments is welcome.”
Cross consultation was taken from psychiatry i/v/o schizophrenia
35 year old male came to the casuality on 21/12/2021 at around 12 am with chief complaints of
fever since 4 days. Shortness of breath since today afternoon
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 4 days back then he developed . Fever since four days , which was insidious onset , intermittent high grade associated with chills and rigor .
SOB since one day sudden in onset rapidly progressive from class 3-4 according to NYHA classification .
No H/O cough, cold, soar throat
No H/O Abdominal Distension, pain abdomen ,nausea, vomitings , loose stools
No H/O Pedal Edema ,facial puffiness, orthopnea and PND.
No H/O burning micturition , decrease urine output, frothy urine ,polyuria , polydipsia , polyphagia
No H/O Fall, LOC, seizures, trauma to head/ chest
PAST HISTORY
History of schizophrenia diagnosed at the age of 15 years. Patient had complaints of auditory and visual hallucinations started on tab risperidone 2mg ,patient was non complaint to treatment . Relapses + . Currently patient was on tab OLANZAPINE 10mg since 2 years.
No history of DM,HTN,Asthma,Epilepsy,CAD,TB
No history of similar complaints in the past.
PERSONAL HISTORY
Diet-Mixed
Appetite-normal
Bowel & Bladder-Regular
ADDICTIONS :
He consumes alcohol occasionally (90 ml since 10 years )
Non-smoker
GENERAL EXAMINATION
Patient was conscious,tachypenic and irritable with Glasgow coma scale of E4V3M6. Pupils were normal in size and bilaterally reacting to light.
Was moderately built and nourished
Dehydration +
No pallor,icterus, cyanosis, clubbing, lymphadenopathy
VITALS ON ADMISSION
Temp – afebrile
BP-90/60 mmhg
PR-92bpm regular, normal volume
RR-32cpm
Spo2-88% on RA, 98% with 8L of o2
GRBS- 454 mg/dl
JVP: normal
SYSTEMIC EXAMINATION
CNS EXAMINATION:
GCS – E4V3M6
TONE: Normal in all 4 limbs
RIGHT LEFT
REFLEXES: Biceps 2+ 2+
Triceps 1+ 1+
Supinator 1+ 1+
Knee 2+ 2+
Ankle 2+ 2+
Plantars mute mute
Corneal Reflex – Present on both sides
Conjunctival Reflex – Present on both sides
Neck Rigidity – absent
Brudzinskis sign : absent
Kernigs sign: absent
RESPIRATORY SYSTEM:
Upper Respiratory Tract: Normal
Lower Respiratory Tract:
Bilaterally symmetrical
Trachea – Central
Respiratory movements appeared equal on both sides
Palpation:
Trachea position was central
Respiratory movements were equal on both the sides
Percussion:
Dull note present in b/l IAA ,ISA .
Resonant in remaining areas .
Auscultation:
Bilateral equal airway entry present
Bilateral inspiratory crepts present in IAA,ISA areas .
CARDIOVASCULAR SYSTEM:
Inspection:
Symmetrical chest
No visible sinuses, scars, pulsations, precordial bulge
Palpation:
Apex beat present in 5th Intercostal space, 1 cm medial to Midclavicular line
Auscultation:
S1,S2 heard
No murmurs .
PER ABDOMEN:
Inspection:
Shape of the abdomen – Scaphoid
Umbilicus – inverted
No visible scars, dilated veins
Palpation:
Diffuse Tenderness in all areas
No organomegaly
Auscultation:
Bowel sounds present
No bruit heard
PROVISIONAL DIAGNOSIS
? DIABETIC KETOACIDOSIS
DENOVO DM - 2
RESPIRATORY DISTRESS SECONDARY TO METABOLIC ACIDOSIS
? VIRAL PNEUMOUNIA
H/O SHIZOPHRENIA
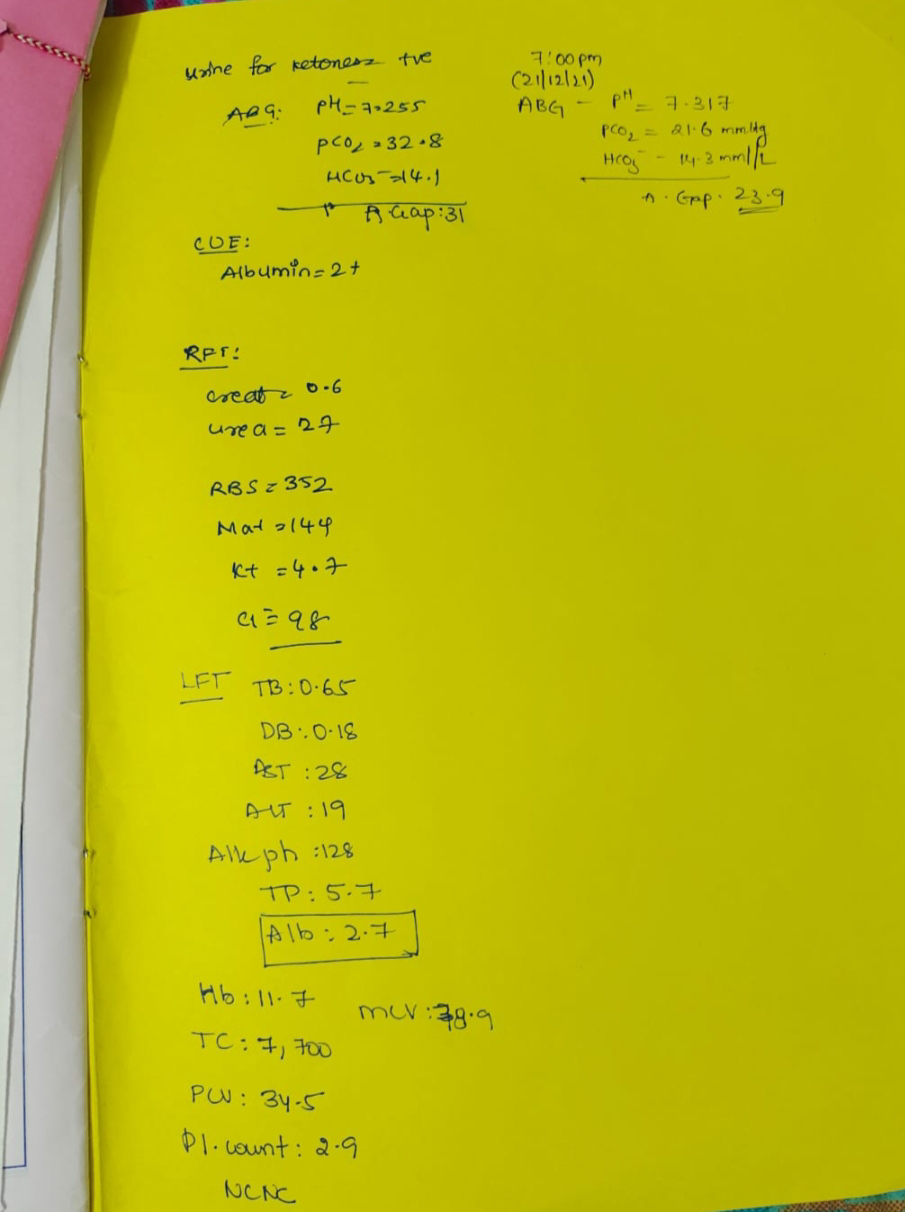
INVESTIGATIONS
Serology - HbsAg +ve
Dengue - negative
Blood for M.P strip test - negative
FINAL DIAGNOSIS
DIABETIC KETOACIDOSIS , DENOVO DM-2 ,SEVERE METABOLIC ACIDOSIS , ? VIRAL PNEUMONIA TYPE 1 RESPIRATORY FAILURE , SCHIZOPHRENIA,HbsAg +ve
TREATMENT
1)HEAD END ELEVATION
2) O2 Inhalation to Maintain spo2>=94%
3)IVF – 0.9%NS 1L FOR 1ST hour
1L FOR 2ND hour
1L FOR 3rd hour
4) IVF – 0.9% NS @ 250ml/hr for next 6 hours
5)INJ. HAI – 0.1IU /KG /B.wt IV /STAT f/by
6) INJ.HAI – 1ml in 39ml NS @ 6ml/hr infusion (according to ALGO 1 )
7) INJ. PANTOP 40mg IV/OD
8)INJ.ZOFER 4mg IV/SOS
9) INJ.AUGMENTIN 1.2gm IV /BD
10) NEB WITH BUDECORT-12th hourly,IPRAVENT-6th hourly
11)GRBS and BP monitoring hourly
12) BIPAP - intermittently
At around 10 am on 21/12/21 ,as the patient MAP >=65mm of Hg was not maintaining . Patient was started on inj NA 2amp in 46 ml NS@6ml/hr through femoral catheter .
DEATH SUMMARY
32 year old male came with complaints of fever since 5 days with sob since yesterday afternoon o/e temp - 99 F , BP - 90 /60 mm hg, PR- 120 BPM, RR- 32 CPM, sp02 - 98 % with 8L of o2 , ABG showing metabolic acidosis with high blood sugar with Ketone bodies positive, provisional diagnosis as DKA with Denovo DM with severe metabolic acidosis ? viral pneumonia ,h/o schizophrenia 10 years on medication(intermittent )patient was started on INJ HAI 40 units ml in 40 ml ns started infusion @ 6 ml /hr with IVF ns @250 ml /hr .Patient was put on bipap and ionotropic support to maintain MAP >= 65mm of hg .
Patient became drowsy ,tachypnic,sp02 was falling down at around 5:30PM on 21/12/21 patient was intubated and connected with mechanical ventilator and later patient had sudden cardiac arrest with absent central and peripheral pulse .
CPR was initiated according to 2020 AHA guidelines , CPR continued for 30 min .
Despite of all efforts and above resuscitation patient could not be revived and declared dead at 7 pm on 21/12/21 .
Immediate cause of death : metabolic acidosis and hypotension secondary to sepsis .
Antecedent cause : Diabetic ketoacidosis with denovo dm , ? viral pneumonia ,type 1 respiratory failure , h/o schizophrenia .








Comments
Post a Comment